The Medical War
British Military Medicine in the First World War
Mark Harrison
2010
The First World War is notorious for demonstrating the devastating effects that follow when industrialised nations commit to total war with each other. It is among the bloodiest wars thus far in human history, only eclipsed two decades on by World War II, and has shaped international relations in the century since. The world was introduced to chemical weapons, military aircraft, and mechanised tanks, but alongside these offensive innovations was the beginning of what we might call modern medicine applied to the battlefield.
The Medical War by Mark Harrison is an account of the various organisational and logistical challenges faced by the Army Medical Services, and by extension the Royal Army Medical Corps, over the course of World War I. He begins with the early stages of the Western Front, detailing the lack of resources and reliance on volunteers and donations, to the development of the casualty clearing stations and sophisticated means of load balancing. He then goes on to discuss the ill-fated fronts in Salonika, Gallipoli, Mesopotamia and East Africa, and their struggles against the natural enemies of malaria, dysentery, and typhoid.
Accepting the risk of sounding ridiculous, the first thing that strikes is the sheer scale the Great War. The comparatively small No. 30 Casualty Clearing Station (CCS), had ‘just’ 500 beds, approximately the same number as the relatively large district general hospital that I work at, and could be packed up and redeployed in as little as 36 hours.
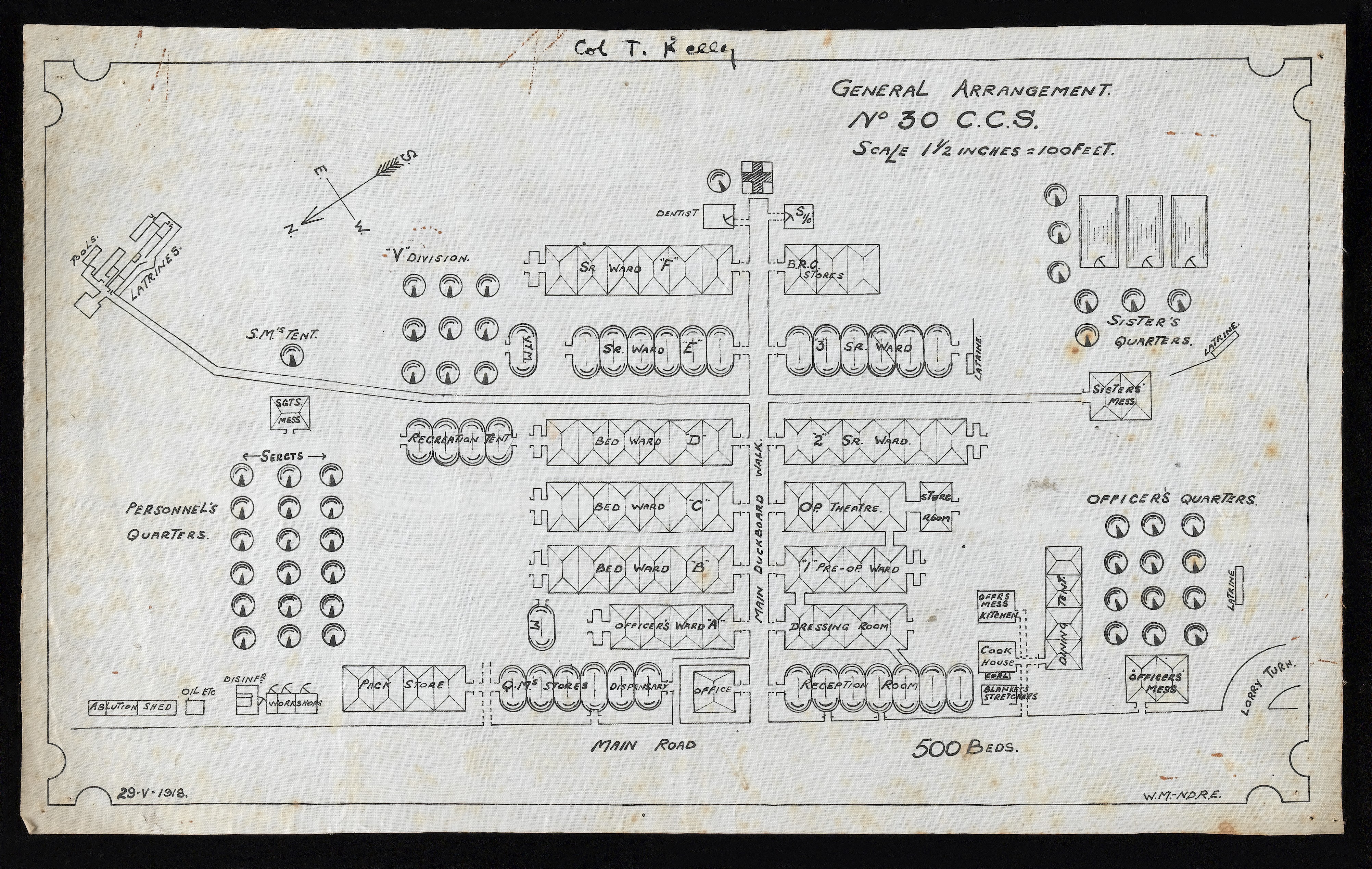
No. 30 Casualty Clearing Station
Layout of No. 30 Casualty Clearing Station operating on the western front. Credit: Wellcome Library L0044173.
The CCS was ideally placed just outside of enemy artillery range and with good railway access to facilitate the evacuation of casualties towards the field hospitals. Their main function was the rapid assessment and triage of incoming wounded from the front, as well as carrying out life and limb saving treatments. As the war went on, the CCS became ever more advanced, being equipped with their own X-ray machines and surgical teams. Following the battle of Loos, sophisticated methods of casualty disposal were implemented, allowing overburdened CCSs to be relieved by others in their region. This was put to the test during the first month of the Somme offensive, in which around 96,000 casualties were assessed by the 14 CCSs belonging to the 4th Army, a truly astonishing accomplishment under such pressure.
Further emphasising the scale of healthcare resource was the collection of military hospitals at Étaples, which provided beds for approximately 14,000 patients, far beyond the scale of anything existing in the UK today. By the end of the war the total number of beds available for military patients in Britain was over 360,000. Although these include convalescent patients, which are less common today, this figure is more than double the roughly 145,000 beds available for the NHS in 2022.
Aside from the scale of the war, I found it interesting to read about the influence that public and parliamentary opinion had on the conduct of the leading generals and their staff. Erroneously, I would have thought the military establishment relatively immune from the machinations of civilians, yet they were the subject of several semi-public commissions into their various failings. Despite the use of heavy censorship, enough reports and letters reached home mentioning the lack of motorised ambulances and hospital trains to cause a wave of donations and consternation in the press. Field Marshal Haig in particular seems to have viewed medical provision as vital towards the maintenance of morale in the field and at home.
Another area where public opinion held considerable sway was in abdominal injuries. In the early stages of the war they carried an exceptionally grim prognosis, with typical mortality in those reaching a CCS of 80%1, and likely many more died in situ. Lord Lister had published his findings on antisepsis in surgery several decades previously2, and after a rocky start, the medical establishment had accepted his views by the outbreak of war. However, maintaining a clean operating environment close to the front line proved an obvious challenge. Further, in a nod to the dreadful algebra of necessity, one French surgeon wrote:
One abdomen, one laparotomy, means a whole hour devoted to an altogether uncertain result; it means, at most, half a chance of saving one man. An hour given to three other severe wounds means you will save three at least.
Altogether, reports of abdominal cases being set to one side at casualty clearing stations were at risk of generating considerable ill-will, and the War Office implemented an array of changes in the face of this criticism.
By the end of the war the outlook for these patients had changed significantly. Dedicated abdominal surgical centres were created relatively close to the front line. Not only were these home to specialist surgical teams, their forward position reduced the time-to-theatre, decreasing rates of infection. Innovations in the treatment of shock, such as intravenous fluid and transfusion3, also helped to reduce mortality. Furthermore, efforts were made to standardise treatment with the publication of manuals, such as the Oxford War Primers, written through the collaboration of civilian and military medical personnel.
So successful were these centres that by 1918, the recovery rate for abdominal cases reaching them ranged from 66% to 80%. During the war, specialisation took off, spawning dedicated hospitals for orthopaedics, psychiatry, gas injuries, and many more.
As far as the Western Front appears to have benefited from learned experience, fronts elsewhere appear to have suffered from generals whose techniques belonged to a different era. The campaigns in Gallipoli, Salonika, and Mesopotamia suffered at least initially from leadership which gave little regard for medical arrangements.
The CCSs in Gallipoli had to be set up on various beachheads, and were victims to rifle and artillery fire. There was also a drastic shortage of medical ships to transport casualties to the hospitals at Mudros and Alexandria, and conditions on the few that existed were said to be bleak. Even if you were fortunate enough to have a space on a transport, the trip from the CCS to the ship was fraught with danger, being carried out on unpowered lighters that were commonly raked by rifle fire on their trip out.
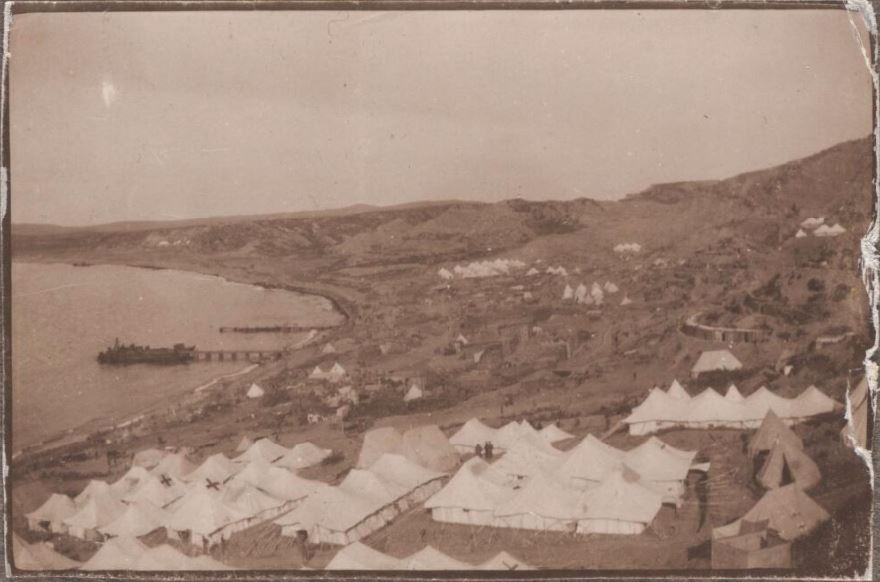
1st Australian CCS
1st Australian casualty clearing station at Anzac, Gallipoli in 1915. Credit: David Izatt, National Library of Australia 736307
The forces also experienced drastic water shortages on the peninsula, with the majority needing to be supplied from supporting ships, which often faced difficulties. Basic hygiene and sanitation suffered as a result, causing waves of dysentery and typhoid. Over the course of the campaign roughly 110,000 casualties were evacuated due to sickness, which compares to almost 125,000 allied soldiers who were wounded by enemy action, not including deaths.
In the East a perpetual battle was waged against malaria. There were some successes, notably in Palestine, where drainage efforts around British bases deprived mosquitoes of their larval incubators. However, when the front advanced further up, a fresh wave of cases would ensue. They were limited by the technology of their time, this being prior to the development of the insecticide DDT, and before the creation of synthetic antimalarials used in prophylaxis today.
However, they did have access to quinine, and used it not only to treat malaria, but as a prophylactic. Quinine has a long history of use in the treatment of fevers, first introduced to Europe in the form on cinchona bark from Peru in the 17th Century. Regrettably, although effective for treatment many forms of malaria, quinine is unable to act as a preventative. When the body is first inoculated by the infected mosquito, the causative plasmodium resides within liver cells, emerging into the bloodstream after a period of days. Quinine is only effective against the malarial parasites after this emergence has occurred, and therefore after infection has started4.
Therefore, quinine apparently had some use in treating the symptoms of malaria, and potentially in keeping some portion of soldiers fit for duty, but was unable to prevent the high degree of ‘wastage’ seen in forces stationed in malarial hotspots. One commander of British forces in East Africa stated that two days of field duty could reduce the effective strength of a regiment by as much as 50%. Further, in the weeks prior to the armistice with Turkey, just under half of the 40,000 British Forces in the area were hospitalised with malaria. It appears that some theatres were decided as much by which side could keep a body of men healthy in an area, than by individual skirmishes and battles.
Efforts towards improving sanitation developed considerably compared to previous wars, such as in South Africa and Crimea. Most regiments had dedicated sanitation units, and officers were given responsibility for maintaining the hygienic practices of men under their command. There were also several successes in preventative medicine, such as vaccination against typhoid and paratyphoid, which although not offering complete protection, considerably improved matters. Interestingly, these vaccines never became officially compulsory, although coercion does appear to have been employed.
Vaccination was opposed by members of the British Union for the Abolition of Vivisection on various grounds, who campaigned via the Daily Mail and directly distributing pamphlets to troops. Their secretary remained a proponent of the miasma theory of disease, in defiance of germ theory, writing opinion pieces ridiculing the concept of bacterial infection. They peddled myths regarding vaccination including that it would trigger its own disease, was developed through animal vivisection, and could cause sexual impotence. There was also a sense that compulsory vaccination was a paternalistic step too far, although the decision not to enforce vaccination also met with considerable resistance from the medical establishment. Some of these arguments seem eerily familiar towards more recent debates regarding COVID-19 vaccination.
Nevertheless, efforts to suppress and prevent disease were drastically more successful than in previous wars. For every one death due to wounds, there were 0.68 deaths due to disease and sickness in the First World War, which compares to two in the South African War, and five in the Crimean War. The conflict marks an interesting point in medical history where new practices and treatments were able to radically change the course of victory.
My aim in writing this is not to give the condensed version of The Medical War, but to discuss some of the aspects that I, naive to most military history, found the most surprising. Harrison also writes fascinatingly regarding venereal disease, the treatment of colonial forces, the differences between enlisted men and officer classes, shell shock, and the relationships between volunteer forces and the army. As on overview of medicine in the First World War, I can’t fault it. Quite frankly, the book is worth it for the bibliography alone, which is evidence to the amount of scholarship involved in its creation. I would say that this is a historians account, therefore emphasises the logistical and military aspects of care, whereas an examination of the medical techiniques used would also be interesting, but would be a separate book entirely.
Overall, I can wholeheartedly recommend it to anyone interested in military medical history, and eagerly await reading Mark Harrison’s account of medicine in the Second World War, Medicine & Victory, which is currently sat on my desk.
-
Cuthbert Wallace, C.M.G., A study of 1200 cases of gunshot wounds of the abdomen, British Journal of Surgery, Volume 4, Issue 16, January 1916, Pages 679–743, https://doi.org/10.1002/bjs.1800041608 ↩︎
-
Lister J. ON THE ANTISEPTIC PRINCIPLE IN THE PRACTICE OF SURGERY. The Lancet. 1867;90(2299):353-356. doi:10.1016/S0140-6736(02)51827-4 ↩︎
-
Aymard JP, Renaudier P. Blood transfusion during World War I (1914 - 1918). Hist Sci Med. 2016;50(3):353-366. ↩︎
-
Shanks GD. Historical Review: Problematic Malaria Prophylaxis with Quinine. Am J Trop Med Hyg. 2016;95(2):269-272. doi:10.4269/ajtmh.16-0138 ↩︎